In March 2020 the SARS-CoV-2 global pandemic was picking up steam. Federal and state advice was being updated daily. Ruby Princess cases had been detected locally by my host GP clinic. Telehealth items had been introduced to the Medicare Schedule, and were starting to predominate GP clinical work. However there was still a need to see patients face to face where examination was deemed necessary.
With such a rapid shift to telehealth, no specific processes had been put in place to reduce risk of face-to-face encounters. I developed the following pandemic response plan, which was accepted and implemented by the GP clinic I was working for.
All patients would start with a telephone appointment. If it was determined after detailed history that the appointment needed to be converted to face-to-face, then a time would be made for the patient to attend. The specific indication for attendance was recorded and a conditional plan was prepared ahead of time.
The waiting room was converted into the "dirty" area of the clinic where everything was assumed infectious. All patients arriving at the clinic were greeted and temperature-checked by a nurse in full PPE.
If the patient was attending for a nurse-led intervention such as injection, wound care, or ECG, they would be directed to a makeshift treatment room at one end of the waiting room. If they needed to be examined, the doctor would don PPE and then see the patient in a makeshift consulting room attached to the waiting area.
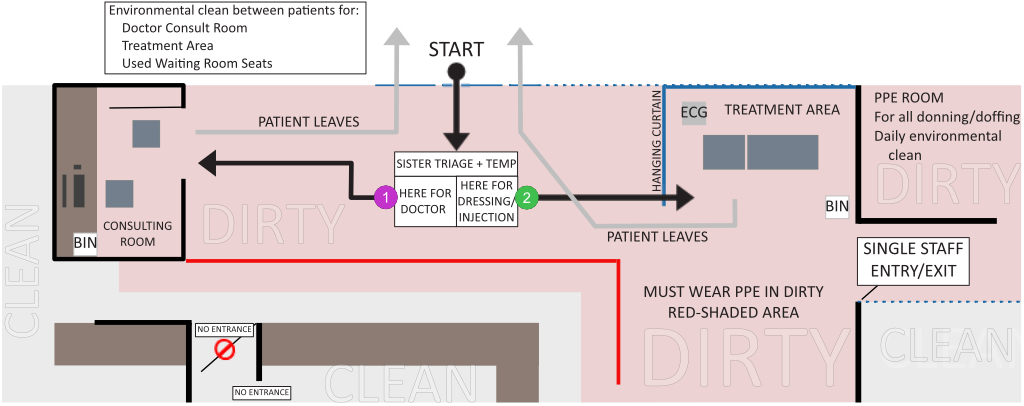
Additional protocols were prepared for donning and doffing of PPE, environmental cleaning requirements, and emptying of dirty area bins.